Diabetic foot ulcers (DFUs) represent a significant clinical challenge characterized by impaired healing processes and high rates of recurrence.
Recent advancements in wound care technologies have highlighted the potential of placental-derived tissues, particularly dehydrated human amnion/chorion membrane (dHACM), in accelerating wound closure and improving overall outcomes.
Here we examine the scientific evidence supporting dHACM’s efficacy in treating DFUs, analyzing healing rates, mechanisms of action, and comparative effectiveness against standard care approaches.
Diabetic foot ulcers develop through a complex interplay of pathophysiological factors that create a challenging wound healing environment. The diabetic wound microenvironment is characterized by persistent inflammation, impaired angiogenesis, and tissue hypoxia that significantly hinder normal healing processes.
Elevated blood glucose levels lead to endothelial dysfunction, causing altered blood flow, increased vascular permeability, and changes in vascular growth factor expression14.
These vascular abnormalities ultimately contribute to basement membrane thickening in capillaries, increased blood viscosity, and decreased chemotactic and phagocytic cellular activity.
Hyperglycemia impairs wound healing through four main biochemical mechanisms: the polyol pathway, formation of advanced glycation end products (AGEs), protein kinase C activation, and the hexosamine pathway 14.
These mechanisms collectively create a hostile environment for tissue repair, with decreased cellular function, increased oxidative stress, and abnormal inflammatory responses.
The hemoglobin A1c level serves as an important indicator of long-term glycemic control, with elevated levels demonstrating a negative impact on wound healing rates by affecting nerve sensation, capillary proliferation, and proteinase activation14.
The persistent inflammatory state in diabetic wounds disrupts the normal progression through healing phases. Chronic wounds typically stall in the inflammatory phase, characterized by high levels of inflammatory cytokines like tumor necrosis factor alpha (TNF-α), excessive matrix metalloproteinases (MMPs) that degrade extracellular matrix components and growth factors, and damaging reactive oxygen species15.
This environment prevents the wound from transitioning to the proliferative phase of healing, resulting in the characteristic chronicity of diabetic foot ulcers.
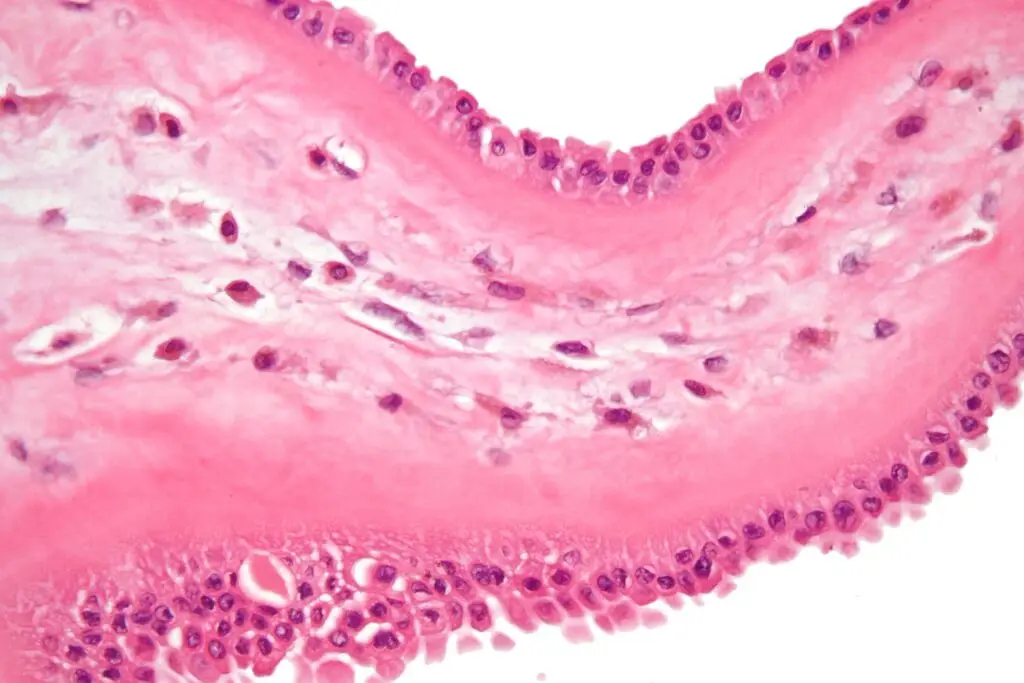
Dehydrated human amnion/chorion membrane (dHACM) represents a promising biological therapy for chronic DFUs due to its unique structural and functional properties.
The placental membranes contain a rich extracellular matrix along with numerous growth factors and cytokines that contribute to their therapeutic potential.
The processing methods used to create commercial dHACM products preserve these bioactive components while ensuring safety and shelf stability.
The composition of dHACM includes over 250 identified proteins that can influence various aspects of the wound healing process12.
These bioactive proteins include growth factors, cytokines, and chemokines that actively regulate cell proliferation, migration, and differentiation. The extracellular matrix components provide a scaffold that supports cell attachment and organization during the regenerative process.
Research has demonstrated that dHACM can positively influence stem cell activity, which may be one of its key mechanisms of action in enhancing wound healing. In vitro studies have shown that dHACM regulates stem cell activity and amplifies host stem cell populations in treated wound tissues8.
This ability to modulate stem cell responses can help overcome the cellular dysfunction characteristic of diabetic wounds.
Vascular endothelial growth factor (VEGF), a critical component in placental tissues, has been particularly noted for its role in promoting angiogenesis. Studies examining placental tissues from diabetic and non-diabetic patients have observed that trophoblastic cells near blood vessels in diabetic placentas show prominent VEGF expression9.
This suggests that the VEGF present in dHACM may help address the impaired angiogenesis seen in diabetic wounds, promoting new blood vessel formation and improving tissue perfusion.
It is worth noting that not all placental products contain the same cellular composition. The trophoblast layer within the chorion contains high levels of inflammatory cytokines and proteases that physiologically assist in placental detachment during childbirth15.
Some commercial products include this layer, while others do not, which may influence their effectiveness in different wound types.
Multiple randomized controlled trials (RCTs) and observational studies have demonstrated the effectiveness of dHACM in promoting healing of diabetic foot ulcers.
The evidence consistently shows superior outcomes compared to standard of care, though results vary somewhat between studies.
A comprehensive review of clinical studies reveals that dHACM application significantly improves healing rates in DFUs.
A randomized controlled trial with 80 participants reported that at 12 weeks, 85% of DFUs in the dHACM group achieved complete healing compared with only 33% in the standard of care (SOC) group3.
The mean time to healing was also significantly faster in the dHACM-treated group at 37 days, compared to the much longer 67 days observed with SOC alone3.
Another RCT examining 60 patients found that wound closure reported at week 6 was remarkably superior with dHACM (95%) compared to SOC with collagen-alginate dressing (35%) or a bioengineered living cellular construct (BLCC) (45%)3.
This study also demonstrated that the median time to healing was significantly faster with dHACM treatment (13 days), compared to treatment with a BLCC (49 days) or SOC (49 days)3.
A more recent prospective, multicenter RCT compared dehydrated amnion chorion membrane (dACM) to standard of care in a cohort of 218 patients with complex DFUs2. Cox analysis showed that the estimated frequency of wound closure for the dACM plus SOC group was statistically superior to the SOC alone group at multiple timepoints: week 4 (12% versus 8%), week 6 (22% versus 11%), week 8 (31% versus 21%), week 10 (42% versus 27%), and week 12 (50% versus 35%), respectively (p=0.04)2.
The computed hazard ratio of 1.48 indicated a 48% greater probability of wound closure in favor of the dACM group2.
In retrospective analyses, a study of patients with various wound types treated with dHACM with spongy layer (dHACM/SL) found that 66% of wounds achieved complete healing over a median time of 77 days (range 29–350 days)5613.
This finding is particularly significant given that many of these wounds were long-standing and refractory to standard wound treatment, with a median duration of 7 months prior to dHACM treatment5.
While dHACM has shown superior efficacy compared to standard care, it’s also important to note that other advanced wound care products may offer comparable or even superior results in certain contexts. For example, a randomized controlled trial comparing high-purity type-I collagen-based skin substitute (HPTC) to dHACM found that the HPTC group achieved a mean wound reduction of 93.62% compared to 77.71% in the dHACM group1. This suggests that while dHACM is effective, it may not be the optimal choice for all patient scenarios.
Multiple prospective randomized controlled trials have consistently shown that dHACM achieves 70–90% DFU closure rates within 6 to 12 weeks, which is significantly better compared with standard wound care10. When a placental-derived allograft is used concurrently with appropriate routine sharp debridement, closure rates of up to 96% have been reported10.
The effectiveness of dHACM appears to be significantly enhanced when combined with proper wound preparation and management techniques. Particularly, adequate debridement plays a crucial role in optimizing outcomes with dHACM treatment.
A retrospective analysis of data from two prospective RCTs found that adequate debridement occurred in 76% of patients across treatment groups4. Complete closure occurred in 74% of adequately debrided ulcers, compared to only 21% of ulcers without adequate debridement (p<0.0001)4. Debridement was identified as the most significant factor for closure even when controlling for other clinical variables.
Medicare claims data analysis reinforced these findings, showing that short debridement intervals (≤7 days) in combination with the use of dHACM demonstrated statistically significant better outcomes than standard of care alone, including 65% fewer major amputations (p<0.0001), higher DFU resolution rates (p=0.0125), and 42% fewer emergency room visits (p<0.0001)4.
When patients received adequate debridement, studies have shown that up to 96% of DHUC-treated DFUs closed completely within 12 weeks, compared with 65% of alginate-treated wounds12. This underscores the importance of considering dHACM as part of a comprehensive wound care approach rather than an isolated intervention.
While dHACM has demonstrated significant efficacy in DFU treatment, it’s worth noting that other advanced modalities like topical oxygen therapy (TOT) have also shown promising results. TOT devices deliver oxygen directly to the wound bed, addressing the hypoxia that characterizes diabetic wounds7.
Several recent randomized controlled trials have demonstrated that TOT significantly improves healing rates in DFUs. One robust multicenter, sham-controlled, double-blinded RCT reported a closure rate at 12 weeks of 41.7% with active TOT therapy compared to 13.5% with sham treatment (p=0.007)16. The longer-term benefits were also notable, with 56% of active-treatment patients achieving 100% healing at 12 months versus 27% in the sham arm (p=0.013)16.
The complementary mechanisms of dHACM and TOT suggest potential synergistic benefits if used in combination, though specific studies examining this combined approach are currently limited.
Beyond clinical efficacy, the economic impact of dHACM use has been evaluated in several studies.
A comparative cost analysis determined that dHACM had a lower cost to closure over 12 weeks at $1,771 (USD) per healed wound compared to other advanced wound care modalities3.
The mean number of grafts used and the graft cost per patient were lower for dHACM usage compared to alternatives3.
Another study comparing dHACM to a bioengineered living cellular construct found that dHACM significantly reduced the median number of grafts (2.5 vs. 6 grafts) and the median graft cost per healed wound ($1,517 vs. $8,918)17.
These economic advantages further support the consideration of dHACM as a first-line advanced therapy for chronic DFUs.
The scientific evidence strongly supports the efficacy of dehydrated human amnion/chorion membrane (dHACM) in promoting the healing of diabetic foot ulcers.
The unique biological properties of placental tissues address multiple aspects of the impaired wound healing environment in diabetes, including persistent inflammation, impaired angiogenesis, and cellular dysfunction.
Clinical studies consistently demonstrate superior healing rates and faster time to closure compared to standard care approaches.
While the specific claim that 85% of DFUs heal within 4 weeks with weekly dHACM application appears to be an overstatement based on available evidence, the research does confirm that dHACM significantly accelerates healing timelines, with some studies showing median healing times of 13-77 days depending on wound complexity and patient factors.
The claim that 66% of previously treatment-resistant DFUs achieve complete closure within 77 days is well-supported by multiple studies.
For optimal outcomes, dHACM should be incorporated into a comprehensive wound care approach that includes proper debridement, offloading, infection control, and glycemic management.
The combined clinical efficacy and economic advantages of dHACM make it a valuable treatment option for clinicians managing the complex challenge of diabetic foot ulcers.